Diseases of the external genitalia are the most common aggressive pathology today. For example, HPV infection can be asymptomatic and have serious consequences for a long time. Certain strains of the virus can lead to cancer of the rectum, vagina, and cervix. Therefore, it is important to diagnose and start proper treatment in a timely manner.
What is HPV?
Human papillomavirus is a common infection of the genitals. This pathogen is found in almost every sixth inhabitant of the planet. When infected, the pathogen enters the epithelial cells, disrupting the division process, which activates the development of various diseases. The virus mostly infects the organs of the urogenital system, the anorectal region. Diseases associated with HPV infection:
- Development of genital warts.
- Development of papillomatosis of the respiratory tract.
- Reproduction of the genitals with the development of a tumor process.
Almost 70% of the population carries the pathogen without clinical manifestation of the disease. Re-infection is also possible during life. Because not everyone who has had a papillomavirus infection develops resistance to the virus.
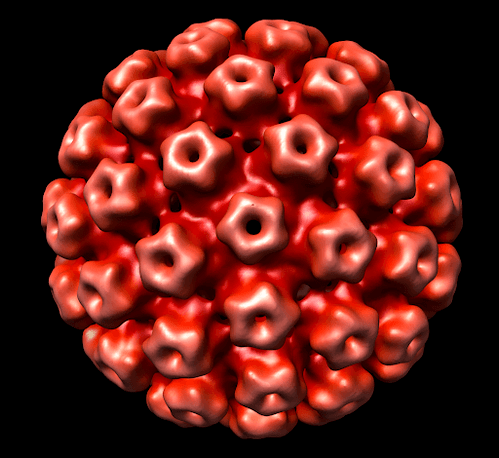
HPV types
More than 100 types of HPV are currently known. Some are relatively safe for human health, while others may activate the development of the oncological process. Most often, the clinical symptoms of the disease do not appear in the early stages. Usually, the first symptoms appear after the onset of provocative factors.
According to oncological activity, such viruses are classified into:
- Strains with high oncogenic risk (18, 16, 31, 33, etc. )
- Low oncogenic risk strains (6, 11, 32, 40-44, 72)
Low oncogenic virus strains lead to the appearance of warts and papillomas on the body surface.
Highly oncogenic strains cause the development of genital warts in the anogenital zone, in the surface of the cervix in women, and in the penis in men.
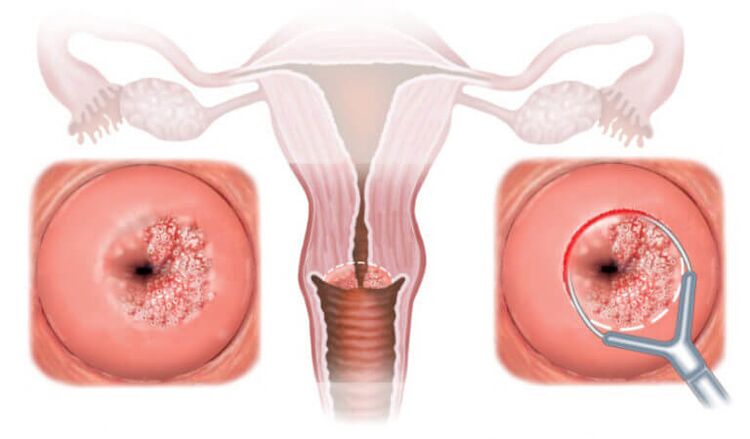
16, 18, 31, 33 long-term effects of the virus on the body can lead to cervical dysplasia and a more frightening disease - cervical cancer.
However, even in the presence of HPV in a body with a high oncogenic risk, oncological pathology does not always develop. Timely appeal to experienced physicians for diagnosis, the right choice of treatment will allow you to never face dangerous clinical manifestations of human papillomavirus.
How to get infected
Both women and men are infected with this pathogen.
The main route of transmission is considered sexual. HPV is usually infected after the first sexual intercourse, but other ways of transmitting the infection are also distinguished:
- Vertical. That is, a newborn can become infected as it passes through the birth canal of an HPV-infected woman.
- Autoinoculation. Self-infection (transfer from one part of the body to another) is possible during epilation or shaving.
- Contact and household. The human papillomavirus remains viable in the environment for some time. Therefore, they can become infected after visiting public places (spa, gym, swimming pool).
- Contact. Possible infection through the wound surface of the skin or mucous membranes (abrasions, wounds, bruises).
- Sexual. The most common route of infection.
Anyone can get a virus infection. In order to diagnose in time, you must undergo preventive examinations with a doctor to determine the first symptoms of the pathology.

The main manifestation of the infection
The presence of papillomavirus infection should not have clinical manifestations for a long time. The incubation period of the disease can take several years, during which the patient can become infected with different types of the virus. Signs of HPV infection can only be observed after exposure to provocative factors (immunodeficiency, hypothermia, stressful situations). In most cases, self-healing of the infection occurs within 1-2 years, but in some patients, the pathology becomes chronic.
The disease can manifest itself in the following formations:
- Genital warts (genital warts). From the outside, these are papillary growths that resemble cauliflower or comb. They are flesh-colored or pink, and may be single or multiple. They can form anywhere, but are most commonly found on the skin and mucous membranes of the genitals. The formations are characterized by low oncogenic potential. They rarely develop into malignancies and usually do not cause discomfort to the patient.
- Flat warts. They have a characteristic structure - they do not protrude above the surface of the mucous membrane of the affected organ. Such formations have a high oncological potential and therefore require a more thorough diagnosis. It is usually located on the mucous membranes of the vagina, urethra, cervical wall. A biopsy is required to diagnose the nature of condyloma.
- Dysplasia. It is characterized by a violation of the differentiated structure of the tissue. The presence of atypical cells that can cause the development of oncological pathology is common.
- Close monitoring and, if necessary, surgical correction is required.



All forms of pathology should be carefully monitored by a physician. To reduce the risk of developing an oncological process, it is recommended to remove such growths on the skin and mucous membranes.
HPV diagnostics
The presence of HPV must be diagnosed intermittently using a variety of physical, laboratory, and instrumental tests.
- Medical examination. It can help identify the presence of warts. When finding genital warts, the cervix should be examined. Ureteroscopy is also possible.
- Colposcopy. Specific tests are performed with acetic acid and iodine solution. They can be used to determine the presence of atypical cells, signs of HPV infection, and cervical cancer.
- Cytological examination. Priest smears are performed on the cervical mucosa. It is a screening test for the presence of cancer-preventing and cancer cells in the wall of the vagina or cervix.
Histological examination of tissues, detection of sexually transmitted diseases, which are often associated with HPV infection, can also be performed. The PCR method has a high diagnostic value. It can be used to identify an HPV strain.

HPV (human papilloma virus) treatment
It is impossible to completely remove the virus from a patient’s body. The doctor can only deal with the consequences of the life of the infectious pathogen. General therapies include symptomatic agents, antiviral agents, and medications that stimulate the immune system.
The following can be used to combat different types of genital warts:
- Cryodestruction, electrocoagulation, laser or chemical cauterization. Such methods are effective in getting rid of genital warts.
- Electrosurgical treatment methods are used to remove the affected area on the surface of the cervix (dysplasia, condyloma).
Prevention of HPV
Various methods are used to prevent the development of the disease. The most effective:
- Monogamous relationships. You only have sex with someone for whom you are the only sexual partner. This method protects itself from all sexually transmitted infections, including HPV.
- Use of barrier contraception. Easy, affordable, but not always 100% safe from infections. The patient can become infected with the virus even if the damaged skin comes into contact with the environment.
- Periodic preventive examinations. Girls should be examined regularly by a gynecologist. This will allow you to recognize the first signs of the disease and start treatment in time.
- Vaccination. An effective and convenient preventive method. Vaccinations can be given to both men and women. The most effective vaccination is before sexual activity (use is allowed from the age of 9). Or persons who are sexually active in the absence of contraindications.
If you suspect the presence of an infection or the first manifestation of the disease, it is important to see a doctor for high-quality diagnosis and timely treatment.























